Electricity could help speed wound healing, new study shows
Electrical impulses may help vessels more quickly get healing agents to injuries
Electric stimulation may be able to help blood vessels carry white blood cells and oxygen to wounds, speeding healing, a new study suggests.
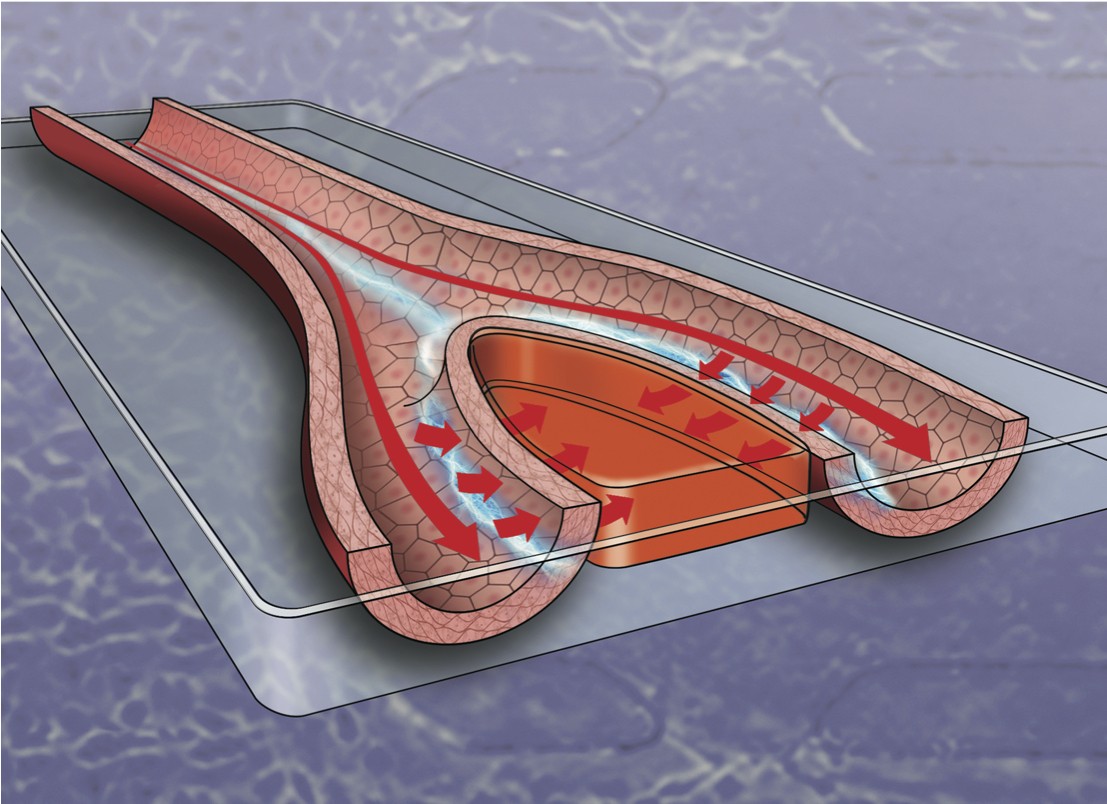
The study, published in the Royal Society of Chemistry journal Lab on a Chip, found that steady electrical stimulation generates increased permeability across blood vessels, providing new insight into the ways new blood vessels might grow.
The electrical stimulation provided a constant voltage with an accompanying electric current in the presence of fluid flow. The findings indicate that stimulation increases permeability of the blood vessel – an important characteristic that can help wound-healing substances in the blood reach injuries more efficiently.
 “There was this speculation that blood vessels could grow better if you stimulated them electrically,” said Shaurya Prakash, senior author of the study and associate professor of mechanical and aerospace engineering at The Ohio State University. “And we found that the response of the cells in our blood vessel models shows significant promise towards changing the permeability of the vessels that can have positive outcomes for our ongoing work in wound healing.”
“There was this speculation that blood vessels could grow better if you stimulated them electrically,” said Shaurya Prakash, senior author of the study and associate professor of mechanical and aerospace engineering at The Ohio State University. “And we found that the response of the cells in our blood vessel models shows significant promise towards changing the permeability of the vessels that can have positive outcomes for our ongoing work in wound healing.”
Blood vessels are crucial for wound healing: They thread throughout your body, carrying nutrients, cells and chemicals that can help control inflammation caused by an injury. Oxygen and white blood cells – which protect the body from foreign invaders – are two key components delivered by blood vessels.
But when there is an injury – for example, a cut on your finger – the architecture of the blood vessels at the wound site are disrupted. That also interrupts the vessels’ ability to help the wound heal. Blood vessels regrow on their own, almost like the branches of trees, without external sources of electricity, as part of the healing process.
“And as the blood vessels begin to grow, they replenish the skin and cells and establish a healing barrier again,” Prakash said. “But our question was: How do you make this process better and faster, and is there any benefit to doing that?”
What they found, in laboratory tests performed using human cells, is that stimulating blood vessels with electricity showed a marked increase in blood vessel permeability, which is a physical marker suggestive of possible new vessel growth.
“These initial findings are exciting, and the next phase of the work will require us to study if and how we can actually grow new vessels,” Prakash said.
 Jon Song, co-author of the paper and associate professor of mechanical and aerospace engineering at Ohio State, said the results imply that one of the primary ways blood vessels work to heal injuries is by allowing molecules and cells to move across the vessels’ walls.
Jon Song, co-author of the paper and associate professor of mechanical and aerospace engineering at Ohio State, said the results imply that one of the primary ways blood vessels work to heal injuries is by allowing molecules and cells to move across the vessels’ walls.
“And now we have better understanding for how electric stimulation can change the permeability across the vessel walls,” Song said. “Let’s say you have a cutaneous wound, like a paper cut, and your blood vessels are severed and that’s why you have blood leaking out. What you need is a bunch of bloodborne cells to come to that place and exit out the blood vessel to initiate the wound repair.”
The study suggested that changes in blood vessel permeability could get those bloodborne cells to a wound site more quickly, though it did not explain the reasons why that happened. The study seemed to indicate that electricity affected the proteins that hold blood vessel cells together, but those results were not conclusive.
The study is an extension of work by a broader team, led by Prakash, that previously showed electric bandages could help stimulate healing in wounded dogs. That work indicated that electrical stimulation might also help manage infections at wound sites – a phenomenon the researchers also hope to research further.
Other Ohio State researchers who worked on this study include Prashanth Mohana Sundaram, Kaushik K. Rangharajan, Tanner J. Hadick and Ehsan Akbari. This work was funded by the National Heart, Lung and Blood Institute, the American Heart Association and the National Cancer Institute.