Study: Drug Could Help Preserve Brain Function After Cardiace Arrest
COLUMBUS, Ohio – An experimental drug that targets a brain system that controls inflammation might help preserve neurological function in people who survive sudden cardiac arrest, new research suggests.
Survival rates for sudden cardiac arrest are low, but recent medical advancements have improved the chances for recovery. Many people who do survive suffer a range of disorders that relate to neurological deficits caused by loss of blood flow to the brain when their heart stops.
The researchers, led by a team at Ohio State University, believe these neurological problems might relate to inflammation and brain-cell death. The study revealed how the brain is damaged during cardiac arrest, as well as how a drug might counter those effects.
 Courtney DeVries
Courtney DeVries
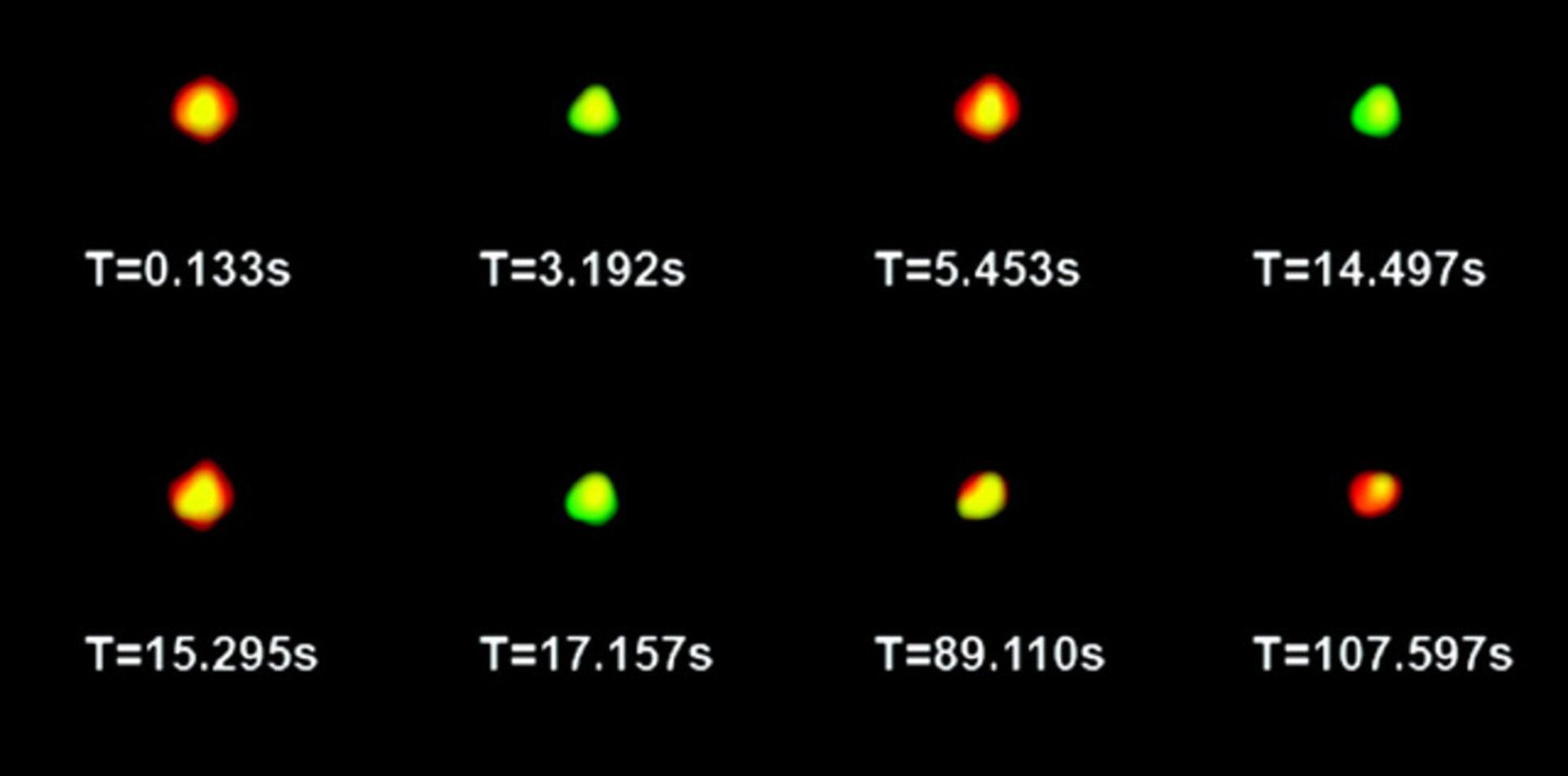
The scientists identified in a mouse model how the loss of blood in the brain sets off a process that attracts inflammatory compounds and kills brain cells. The study showed that these damaging effects were associated with alteration of the cholinergic system – an area of the brain that sends signals using the neurotransmitter acetylcholine to regulate inflammation.
Mice that were treated with an experimental drug called GTS-21, which activates acetylcholine, had lower levels of inflammatory chemicals and reduced damage to brain cells in the days following a surgically induced cardiac arrest and subsequent resuscitation.
“This is a drug that has been used safely in humans in clinical trials, so we think our findings have significant clinical potential,” said Courtney DeVries, professor of neuroscience and psychology at Ohio State University and senior author of the study. “Another very important aspect of the study is that the drug was not given until 24 hours after resuscitation, and yet it was successful at reversing inflammatory effects in the brain. So there would be a large therapeutic window of time if this could eventually be used clinically.”
The research is published in the March 2 issue of The Journal of Neuroscience.
Cardiac arrest is not the same as a heart attack, which occurs when blood flow to the heart is interrupted. In sudden cardiac arrest, the heart’s electrical system malfunctions and blood flow stops altogether. The American Heart Association estimates that fewer than 8 percent of people who suffer cardiac arrest in a home or community setting will survive, and that brain damage can occur within four to six minutes after the heart has stopped. Lasting effects of this brain damage can include physiological problems as well as memory loss and increased anxiety and depression.
In this study, the researchers surgically induced cardiac arrest in groups of anesthetized mice and then revived them eight minutes later using cardiopulmonary resuscitation. The scientists then analyzed brain tissue in mice three and seven days after the heart stoppage. Some mice received the drug beginning 24 hours after resuscitation, and some did not.
Within three days after the cardiac arrest, the untreated animals’ brain tissue showed increased levels of immune cells in the central nervous system that indicate neurons are under attack. In addition, there were signs of high activity in the brain associated with the creation of compounds linked to inflammation.
"One aspect of the study is that the drug was not given until 24 hours after resuscitation, and yet it was successful at reversing inflammatory effects in the brain. So there would be a large therapeutic window of time if this could eventually be used clinically."
These compounds included tumor necrosis factor-alpha, interleukin-1 beta and interleukin-6 (IL-6) – all members of a family of proteins called cytokines, chemical messengers that cause inflammation, most often to fight infection or repair injury. When these proteins are circulating without an infection to fight, the body part hosting them – in this case, the brain – experiences excess inflammation. By day seven after cardiac arrest, some untreated mice also had elevated levels of IL-6 in their bloodstream, a sign that excessive inflammation was present in other parts of the body.
“The higher IL-6 levels in the blood are important, because this cytokine is also a marker of inflammation in humans,” DeVries said.
The researchers also observed reduced activity levels of the enzyme that generates the neurotransmitter acetylcholine, suggesting that chemical signaling that protects the brain by regulating inflammation had been severely altered in mice that had experienced cardiac arrest.
“The cholinergic system is important for maintaining an appropriate balance between inflammation in the central nervous system and throughout the body,” said DeVries, also an investigator in Ohio State’s Institute for Behavioral Medicine Research. “Though the presence of cytokines can be beneficial in limited amounts, the huge inflammatory response in these mouse brains became detrimental to the survival of the neurons.”
Twenty-four hours after cardiac arrest and resuscitation, some of the mice received daily treatments of the experimental drug GTS-21. This drug can reverse these signaling malfunctions and restore the anti-inflammatory properties of the cholinergic system.
Mice that received this treatment had lower levels of pro-inflammatory compounds in their brains three days later and fewer inflammation markers in their blood seven days later than did untreated mice. In addition, fewer brain cells died in these mice compared to mice that did not receive any treatment after cardiac arrest and resuscitation.
When the researchers simultaneously introduced a drug that can counter the GTS-21, the mice showed none of the improvements associated with the treatment.
“This confirmed for us that we were targeting the appropriate system to reduce inflammation in the brain,” DeVries said. “Essentially, what we were trying to do is provide balance to the cholinergic system. GTS-21 replaced a signal that was missing, which in turn reduced the inflammatory response to levels that are not as damaging to neurons.”
DeVries also noted, however, that cardiac arrest disrupts the cholinergic signaling at multiple points. So restoration of one part of the system appears to reduce damaging effects on some, but not all, responses to the blood loss in the brain.
She also said her lab is continuing research in this area to further explore the link between inflammation in the brain that follows cardiac arrest and resulting neurological problems.
“The cognitive effects are one of the biggest patient concerns. If these symptoms are related to increased inflammation that occurs after cardiac arrest, this drug might have potential benefits that go far beyond control of inflammation; they might also help improve other symptoms,” DeVries said.
GTS-21 is currently being tested by other researchers as a potential treatment for Alzheimer’s disease, schizophrenia and nicotine addiction. It can cross the blood-brain barrier, so it can be given intravenously.
This work was supported by the National Institute of Neurological Disorders and Stroke, the National Institutes of Health, the American Heart Association and the J. Parker and Kathryn Webb Dinius Fellowship at Ohio State.
Co-authors include Greg Norman (now at the University of Chicago), John Morris, Holly Brothers and Gary Wenk of Ohio State’s Department of Psychology; Kate Karelina, Zachary Weil and Ning Zhang of Ohio State’s Department of Neuroscience; and Yousef Al-Abed, Valentin Pavlov and Kevin Tracey of the Feinstein Institute for Medical Research at North Shore-LIJ Health System in Manhasset, N.Y.
#
Contact: Courtney DeVries, (614) 292-7353; DeVries.14@osu.edu
Written by Emily Caldwell, (614) 292-8310; Caldwell.151@osu.edu

